Multiple Myeloma (MM) is the second most common hematologic neoplasia, and it remains largely incurable due to the genetic heterogeneity of the patients. We have recently characterized the epigenome of plasma cells from patients with MM, describing the de novo activation of the chromatin as a unifying factor underlying the pathobiology of the MM. Precisely, we identified 1556 de novo active regions, showing the H3K27ac chromatin activation mark, in MM in comparison to different subpopulations of normal B cells. Moreover, those de novo active regions where enriched in Transcription Factor Binding Sites (TFBS). In order to defined the potential role of these regions we have performed a CRISPR-Cas9 screening using guides against 56 TF that presented TFBS in de novo active regions and that are expressed in MM. A CRISPR-Cas9 library containing 10 guides for each gene was transduced in two MM cell lines (MM.1R and KMS-11) and the presences of guides were analyzed at days +1, +14 and +21. Out of the 22 TFs shown to be essential for MM survival, there were 3 members of the IRF TF family (IRF1, IRF2 and IRF5). Single knockdowns identified IRF2 and the previously described IRF4 as the best candidates.
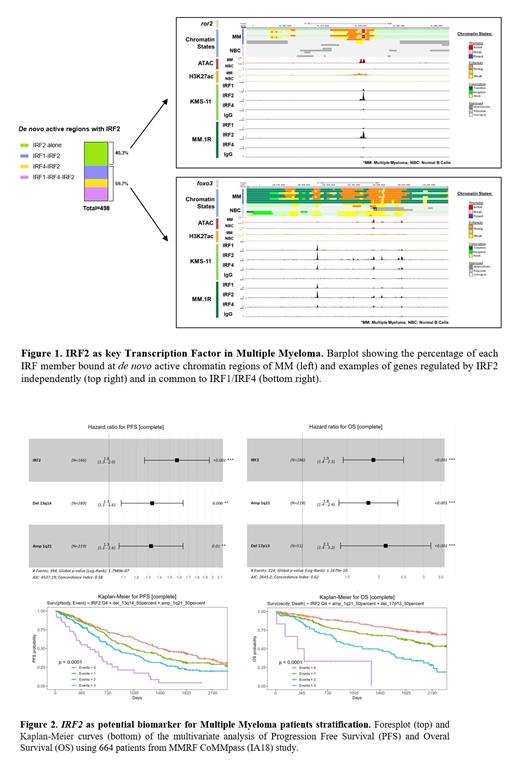
To characterize the signalling pathways involved in IRF family regulation of MM, the chromatin regions where IRF1, IRF2 and IRF4 are bound were mapped using CUT&RUN in MM.1R and KMS-11 cell lines. Interestingly, the three TF were located in 573 out of the 1556 de novo active regions. Notably, IRF2 was present in the 86.9% of those regions, and in 40% of the cases, the binding occurred independently of IRF1 or IRF4 ( Fig. 1). Additionally, the genomic distribution demonstrated that the regions where IRF2 binds alone were enriched in promoters compared to those regions where IRF1 and IRF4 also bound, being these enriched mostly in the gene body. Gene Ontology studies showed that IRF2, as well as IRF1/4 were involved in regulation of cell death in response to oxidative stress, while only IRF2 autonomously was involved in the regulation of pathways relevant for MM such as the kinase dysregulation, cell migration and osteoblast regulation. Furthermore, using our previous RNA-seq data, we observed that the majority of the genes regulated uniquely by IRF2 presented an overexpression in MM in comparison to different subpopulations of normal B cells. This overexpression was already identified in plasma cells from MGUS (Monoclonal Gammopathy of Undetermined Significance) patients and SMM (Smouldering MM) stages in contrast to normal bone marrow plasma cells.
Finally, we examined the impact of IRF2 and IRF4 expression on the outcome of MM using RNA-seq data from 664 patients from MMRF (MM Research Foundation) CoMMpass (IA18) database. We observed that patients with higher expression of IRF2 presented significantly poorer Progression Free Survival (PFS) and Overall Survival (OS) in univariate analysis. Interestingly, in multivariate analyses taking into account the classic high-risk genetic factors for MM, the expression of IRF2 together with del13q and amp1q resulted in a significantly lower PFS (global p < 0.001) and the expression of IRF2 together with amp1q and del17p resulted in statistically significant worse OS (global p < 0.001). On a multivariate model, MM patients were stratified according to the number of events ( IRF2 expression, del13q and amp1q for PFS and IRF2 expression, amp1q and del17p for OS) into four risk groups both for PFS and OS ( Fig. 2).
In conclusion, our study demonstrate that IRF2 plays a significant role in the pathogenesis of MM by participating in the regulation of the de novo active chromatin regions, specifically regions related to kinase pathway. Additionally, IRF2 represents a robust biomarker that in combination with classical genetic markers improves stratification of MM patients. These results establish IRF2 as a promising candidate for new therapeutic strategies in patients with MM.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal